STAYING ON TRACK
The lowdown on handling low blood glucose

How to recognize low blood glucose (hypoglycemia) from diabetes and take action

For most people, low blood glucose (hypoglycemia) is when the amount of glucose in your blood drops below 70 mg/dL. You should ask your diabetes care teamDiabetes care teamYour diabetes care team may include a primary care doctor, a diabetes and hormone doctor (endocrinologist), a registered nurse, a diabetes educator, a dietitian, a heart doctor (cardiologist), a foot doctor (podiatrist), an eye doctor (ophthalmologist/optometrist), a kidney doctor (nephrologist), a dentist, a pharmacist, and a mental health professional. what level of blood glucose is too low for you. Low blood glucose is something that you need to be prepared to treat, so it’s important to know the signs.
What causes low blood glucose?
- Taking certain medicines and eating too few carbohydratesCarbohydrateCarbohydrates are the main kinds of food that raise blood glucose levels. Your digestive system changes carbohydrates into glucose, and then uses this glucose as a source of energy for your cells.
There are 3 main types of carbohydrates in food: starches (complex carbohydrates), sugars (simple carbohydrates), and fiber. Fiber is the part of plant foods, including fruits, vegetables, and nuts, that you can’t digest. (starches)
- Skipping or delaying meals
- Taking too much insulinInsulinA hormone made by the beta cells in the pancreas that helps glucose move from the blood into the cells. Insulin is also an injectable medicine that is used to treat diabetes by controlling the level of glucose in the blood. or diabetes medication (ask your diabetes care team if this applies to you)
- Activity levels higher than usual
- Drinking alcohol without eating enough food
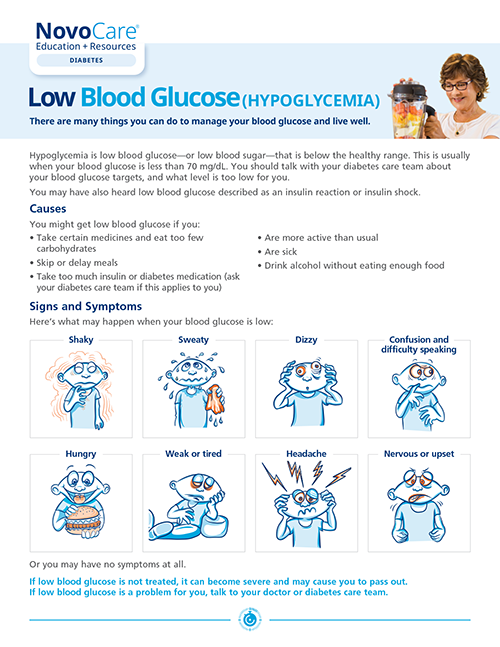
Low blood glucose can happen suddenly and can occur at any time. In most cases, you will notice the signs and symptoms. It’s important to learn to recognize them early, so something can be done before they get worse.
Physical symptoms
The symptoms of low blood sugar may include:
- Feeling clumsy or lack of control over simple movements
- Dizziness or light-headedness
- Rapid heartbeat
- Headache
- Hunger
- Nausea
- Seizure (fits)
- Shakiness
- Sleepiness
- Sweating
- Tingling around the mouth (in the lips or tongue)
- Weakness
Emotional symptoms
- Anxiety
- Personality change (eg, crying for no reason)
- Confusion
- Difficulty paying attention
- Nervousness
- Nightmares or crying out during sleep
Blood sugar should be checked right away if there are any symptoms. If it is low, or if it seems like it might be, follow the “Rule of 15.”
The “Rule of 15” to treat low blood glucose
- Eat or drink food with 15 grams of carbohydrate
- Wait 15 minutes and test blood glucose again
- If it's still low, treat with another 15 grams of carbohydrate
Once your blood glucose returns to normal, help keep it that way by eating a meal or snack, if your next planned meal is more than an hour or 2 away.
What does “15 grams of carbohydrate” look like?
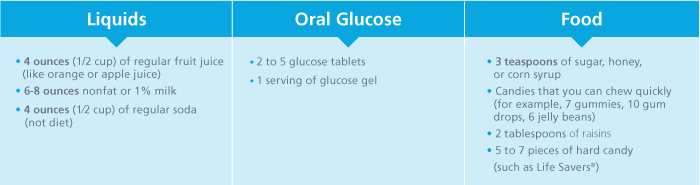
Always check with your doctor about how to treat your low blood glucose. Tell him or her if it often happens. You may need to work together to change your diabetes care plan.
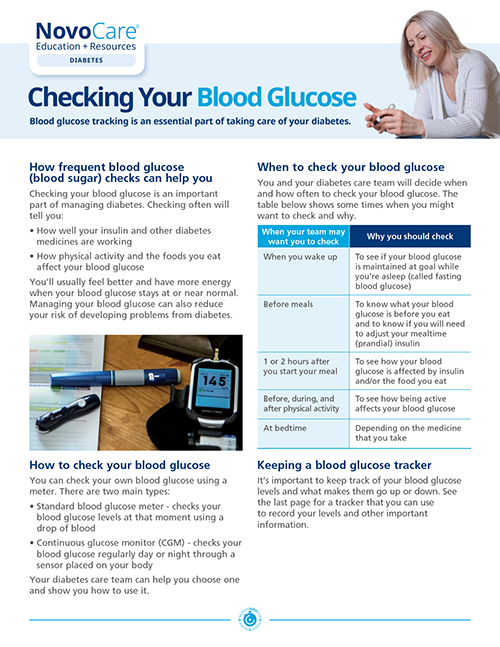
Download Checking your blood glucose

The signs of nighttime low blood glucose include:
- Sweating: Waking up with damp clothes/sheets
- Headache: Waking up with a headache and/or feeling tired, irritable, or confused
- Disturbed sleep: Restless sleep or having nightmares
You may also wake up with a higher blood sugar reading because your body is bouncing back from an overnight low.

Some causes of nighttime low blood glucose:
- Too much activity: Having a very busy day, or being active close to bedtime can decrease blood glucose overnight. For some people, even exercising in the afternoon can lead to nighttime low blood glucose
- Drinking alcohol in the evening: Drinking alcohol, especially in excess, can put you at risk of a lower blood glucose level overnight. Especially if you were drinking on an empty stomach. This is because the liver is busy clearing the alcohol from the blood, instead of making and releasing glucose. If you have type 1 diabetes, drinking alcohol, especially in excess, is generally not recommended
- A late dinner or bedtime: Even if blood glucose is normal before going to bed, having a late dinner (a couple of hours before bed) can cause blood glucose to drop later during the night. You may want to check your blood glucose during the night to see if your results reflect your food intake, physical activity, and insulin doses from the previous day and evening
Avoiding nighttime low blood glucose can mean:
- Not taking too much rapid-acting insulin to correct high blood glucose at bedtime or during the night. It can bring on nighttime low blood glucose. For many people, each unit of rapid-acting insulin can lower blood glucose more at night than during the day
- Evaluating potential risks: Think about all of the causes of nighttime hypoglycemia. If you feel you or the person you care for is at risk, a snack before bed may help, especially if blood glucose levels are already dropping at this time
- Trying an insulin pump: Many people who take insulin are able to reduce their risk of nighttime lows by switching to an insulin pump. If you (or your loved one) are having problems with nighttime low blood glucose and are already using a pump, talk to a doctor about how to adjust the pump’s basalBasal insulinA type of injected insulin that is absorbed slowly and starts to lower blood glucose within 4 to 6 hours after injection. Its strongest effect is 10 to 18 hours after injection depending on the product. This gives the body a low level of insulin to manage blood glucose between meals and overnight. rate to avoid hypoglycemia at night